Part 2 of the “sensory exam” addresses, among other things, QST and how to conduct the test. Feel free to read part 1 before this post.

What do we do in the clinic?
When you have a patient with suspected disc herniation and radiculopathy in front of you, how do you do a sensory exam? Do you use cotton? A pinwheel? Is it enough to just do a screening with light touch of a finger, or is it enough to just ask the patient? I will try to discuss this.
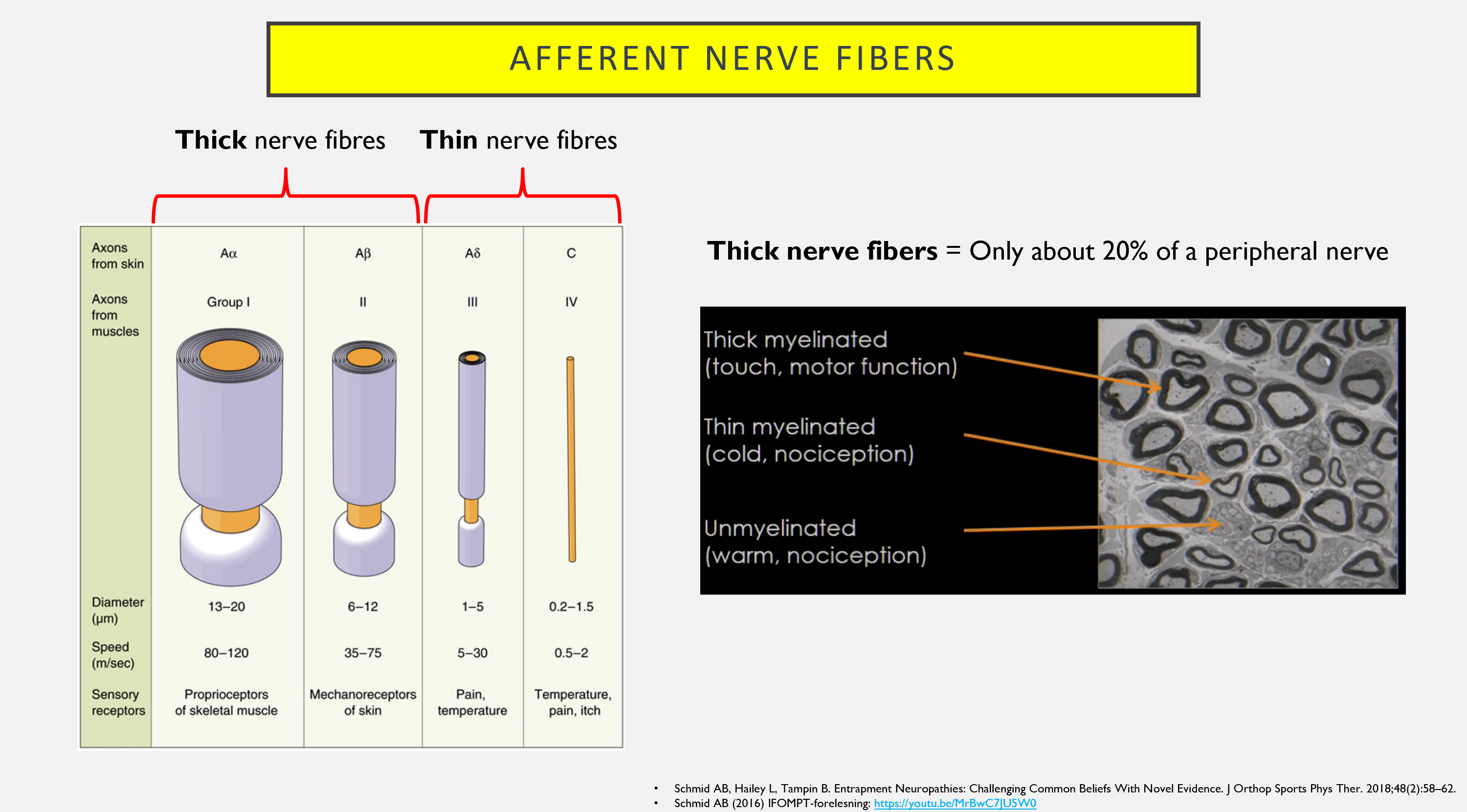
Thick and thin nerve fibers
Traditionally, MSK physiotherapists in Norway have used pinwheels for our sensory exam. Other sources, including Reiman, write that it may be sufficient to test with light touch (1). I somewhat disagree with this. Pricking and light touch test different nerve fibers (2)!
As mentioned in the previous post, previous studies have shown that thick (A-beta) nerve fibers undergo greater deformation compared to thin nerve fibers (A-delta and C-fibers), and according to Frank and Nordin, these are damaged first (3). Newer studies by, among others, Schmid et al. (4) have shown that thin nerve fibers are also affected, perhaps even before the thick nerve fibers. After all, the thin fibers make up 80% of the nerve (5). Therefore, if you are going to conduct a thorough examination of nerve function, you should test both thick and thin nerve fibers (2).
Quantitative Sensory Testing (QST)
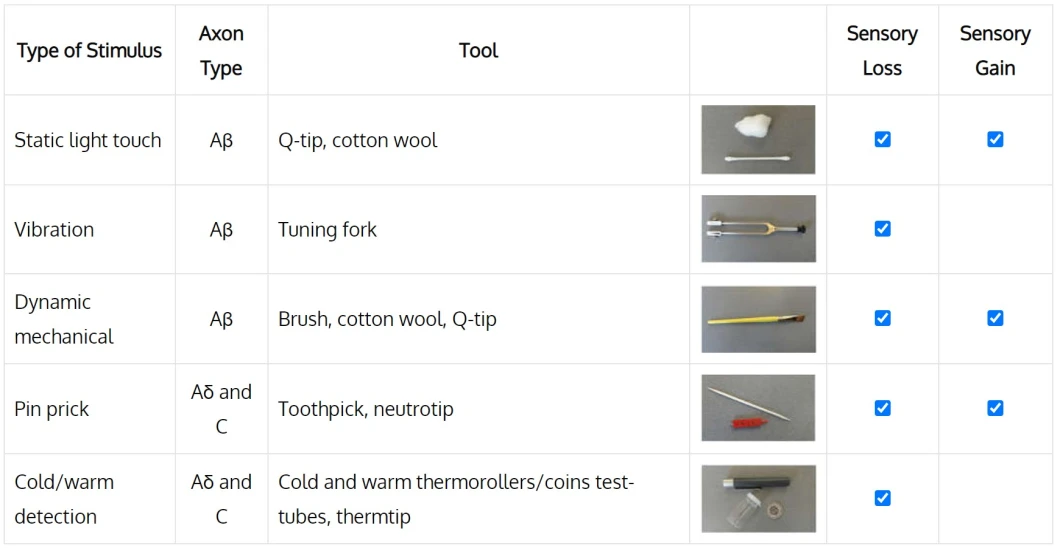
Pinprick and light touch may be sufficient to examine both thin and thick nerve fibers, but you can also supplement with cold/heat, vibration, and “wind-up,” akin to a QST examination (6). QST stands for quantitative sensory testing and is actually a tool used in research or in hospitals, as it requires more advanced equipment (7). However, it has been investigated whether a “cheap version” of QST (bedside quantitative sensory testing) yields almost the same results as the “expensive QST,” and in one study, it has been shown to provide nearly identical results in patients with neuropathic pain (8). This is something that can be done in the clinic.

Light touch
I start by testing light touch with cotton; this tests the thick A-beta fibers. It may be wise for the patient to have their eyes closed during the test. I ask the patient if it feels like increased or decreased sensation or if it feels normal. If there is decreased sensation, the patient indicates in percentage how much compared to the unaffected side. Then I say, “if this side (unaffected side) is 100%, what percentage is this (affected) side?” If both sides are affected, you can find another area, e.g., the upper extremities, and compare with this. If there is pain (allodynia), the area can be marked with a pen, and the patient can indicate pain on NPRS. By marking the area, you can see if it follows a dermatome, a peripheral nerve, or if it is more widespread. This can provide valuable information for clinical reasoning. It may also be that the affected area feels more sensitive without pain; then it is “hyperesthesia.”

Reiman (9) recommends testing light touch with a monofilament – not stroking with cotton/paper, as light stroking with cotton/paper may more be a test for hair and hair follicles instead of skin – especially on the thigh and leg. Alternatively, the cotton ball can be placed gently directly on the skin, so it is not stroked. I would still use cotton, but if the patient is very hairy where it should be tested, it may be wise to use a monofilament instead.
Pinprick
Pinprick tests the thin A-delta and C-fibers (10). In MSK physiotherapy in Norway, this is traditionally tested with a pinwheel. An important point here is that the pinwheel is sharp enough; if not, it does not test the sensation of pricking! I am quite sure that there are several practitioners who test with a pinwheel that is too blunt, and then you can potentially end up testing A-beta fibers instead of A-delta and C-fibers. If you do not have a pinwheel, you can use a needle or toothpick, or you can buy disposable “neurotips.”

It is important to maintain consistent pressure when testing, for example, keep at the same spot on the pinwheel or try to apply the same pressure with the needle. Ask the patient if the prick feels sharp, dull, or if he/she is unsure. It may be wise for the patient to have their eyes closed during the test. Compare with the other side, or another unaffected area if there are bilateral complaints. If there is an area of allodynia, you can test pricking in the surrounding area, as this will evaluate hyperalgesia. If you take a picture with a phone of the marked area of allodynia and hyperalgesia, you can see any changes over time.
Small fibre neuropathy
I think that in principle, it is enough to test pinprick and light touch, as this tests both thin (small) and thick nerve fibers. The thick fibers are also tested by strength tests and reflexes. If you are still unsure whether there may be affection of thin fibers, you can also test cold and heat sensation (A-delta and C-fibers). A negative pinprick, heat, and cold test can exclude affection of thin fibers with high certainty (sensitivity 0.98, specificity 0.20) (11). It has been shown that it can be just as good to do it in the clinic as in a laboratory (12). I usually put the metal part of the reflex hammer under hot or cold water from the tap for a while, dry it off, and test. Others recommend having a coin in your pocket that has been heated up, but who wants to carry a coin in their pocket all the time? It may also be wise to ask in the history if you have changed heat/cold sensation, e.g., if they shower or bathe.
Does there always have to be loss of function?
Be aware that with disc herniation and nerve root affection, there can be both increased (gain) and decreased (loss) function. Previously, I thought that there HAD to be loss of function (hypoesthesia) for there to be nerve root affection, but I now also understand that there can be increased function (4). You may have had a patient with a very positive SLR where you expect decreased sensitivity, but the patient instead has increased sensation in the same leg.
Can you determine if it is disc herniation and radiculopathy by sensory exam? As seen in the chart below, sensory exam alone has a sensitivity of 0.61 and specificity of 0.63 (13).
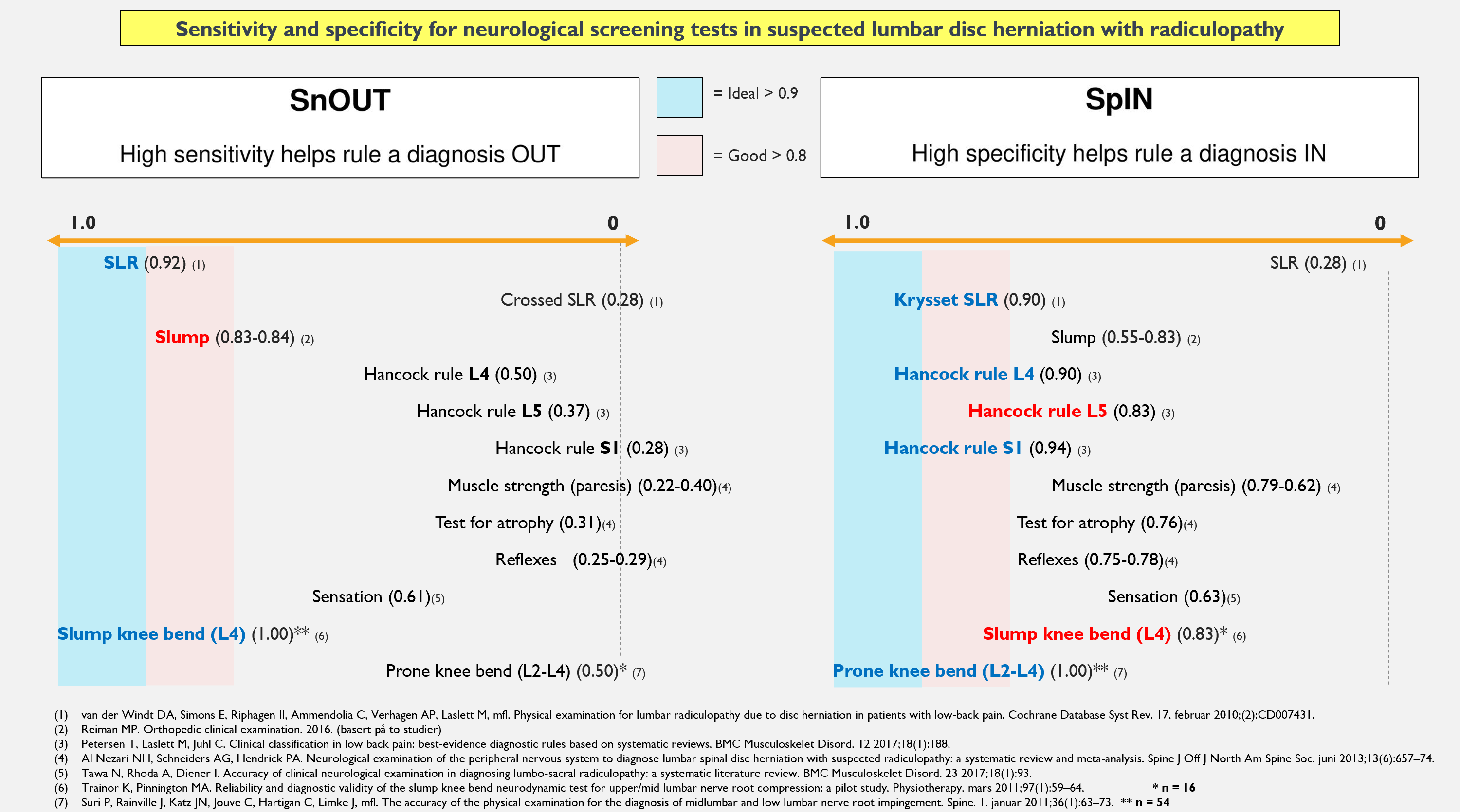
When looking at the studies that have been done, there are some studies that stand out. There are several studies that test against MRI, but only one study that tests against surgery. They write in the review article that sensory exam with pinprick and light touch is very specific and can be used to suggest that there may be radiculopathy (“rule in”) in cases of back pain and radicular pain (13).
Summary
For a comprehensive examination of sensibility, you should test both light touch and pricking. Light touch tests the thick A-beta fibers, while pricking tests the thin A-delta and C-fibers. You can supplement with vibration, cold, and heat (QST), although this is probably not necessary in most cases of disc herniation and radiculopathy. Light touch can be tested with cotton or a monofilament, while pricking can be tested with a needle, pinwheel, or “neurotips.” Make sure the needle is sharp enough.
References
1. Reiman MP. Orthopedic clinical examination. 2016.
2. Schmid AB, Tampin B. Section 10, Chapter 10: Spinally Referred Back and Leg Pain – International Society for the Study of the Lumbar Spine. I: Boden SD, redaktør. Lumbar Spine Online Textbook [Internett]. 2020 [sitert 4. oktober 2020]. Tilgjengelig på: http://www.wheelessonline.com/ISSLS/section-10-chapter-10-spinally-referred-back-and-leg-pain/
3. Nordin M, Frankel VH, redaktører. Basic biomechanics of the musculoskeletal system. 4th ed, international ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins; 2012. 454 s. (Wolters Kluwer Health).
4. Schmid AB, Fundaun J, Tampin B. Entrapment neuropathies: a contemporary approach to pathophysiology, clinical assessment, and management. Pain Rep [Internett]. 22. juli 2020 [sitert 24. september 2020];5(4). Tilgjengelig på: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7382548/
5. Schmid AB, Hailey L, Tampin B. Entrapment Neuropathies: Challenging Common Beliefs With Novel Evidence. J Orthop Sports Phys Ther. 2018;48(2):58–62.
6. Backonja M-M, Walk D, Edwards RR, Sehgal N, Moeller-Bertram T, Wasan A, mfl. Quantitative sensory testing in measurement of neuropathic pain phenomena and other sensory abnormalities. Clin J Pain. september 2009;25(7):641–7.
7. Uddin Z, MacDermid JC. Quantitative Sensory Testing in Chronic Musculoskeletal Pain. Pain Med Malden Mass. september 2016;17(9):1694–703.
8. Buliteanu A, Lazaridou A, Schreiber K, Edwards R, Rajan S, Garcia J, mfl. Validation of a bedside quantitative sensory testing (QST) protocol in chronic neuropathic pain. J Pain. 1. mars 2018;19(3):S52.
9. Reiman MP. Orthopedic clinical examination. 2016.
10. Lind P. Ryggen: undersøgelse og behandling af nedre ryg. 2. utg. Kbh.: Munksgaard Danmark; 2011.
11. Ridehalgh C, Sandy-Hindmarch OP, Schmid AB. Validity of Clinical Small-Fiber Sensory Testing to Detect Small-Nerve Fiber Degeneration. J Orthop Sports Phys Ther. oktober 2018;48(10):767–74.
12. Zhu GC, Böttger K, Slater H, Cook C, Farrell SF, Hailey L, mfl. Concurrent validity of a low-cost and time-efficient clinical sensory test battery to evaluate somatosensory dysfunction. Eur J Pain Lond Engl. november 2019;23(10):1826–38.
13. Tawa N, Rhoda A, Diener I. Accuracy of clinical neurological examination in diagnosing lumbo-sacral radiculopathy: a systematic literature review. BMC Musculoskelet Disord. 23 2017;18(1):93.
